More than 120 confirmed or suspected cases of monkeypox, a rare viral disease seldom detected outside Africa, have been reported in at least 11 non-African countries in the past week. The emergence of the virus in separate populations around the world, in locations where it doesn’t usually appear has alarmed scientists — and sent them racing for answers.
“It’s eye-opening to see this kind of spread,” says Anne Rimoin, an epidemiologist at the University of California, Los Angeles, who has studied monkeypox in the Democratic Republic of the Congo for more than a decade.
The virus is called monkeypox because researchers first detected it in laboratory monkeys in 1958, but it is thought to transmit to people from wild animals such as rodents or from other infected people. In an average year, a few thousand cases occur in Africa, typically in the western and central parts of the continent. But cases outside Africa have previously been limited to a handful that were associated with travel to Africa or with the importation of infected animals. The number of cases detected outside of Africa in the past week alone — which is almost certain to increase — has already surpassed the total number detected outside the continent since 1970,

when the virus was first found to cause disease in humans. This rapid spread is what has scientists on high alert.
But monkeypox is no SARS-CoV-2, the coronavirus responsible for the COVID-19 pandemic, says Jay Hooper, a virologist at the US Army Medical Research Institute of Infectious Diseases in Fort Detrick, Maryland. It doesn’t transmit from person to person as readily, and because it is related to the smallpox virus, there are already treatments and vaccines on hand for curbing its spread. So although scientists are concerned — because any new viral behaviour is worrying — they are not panicked.
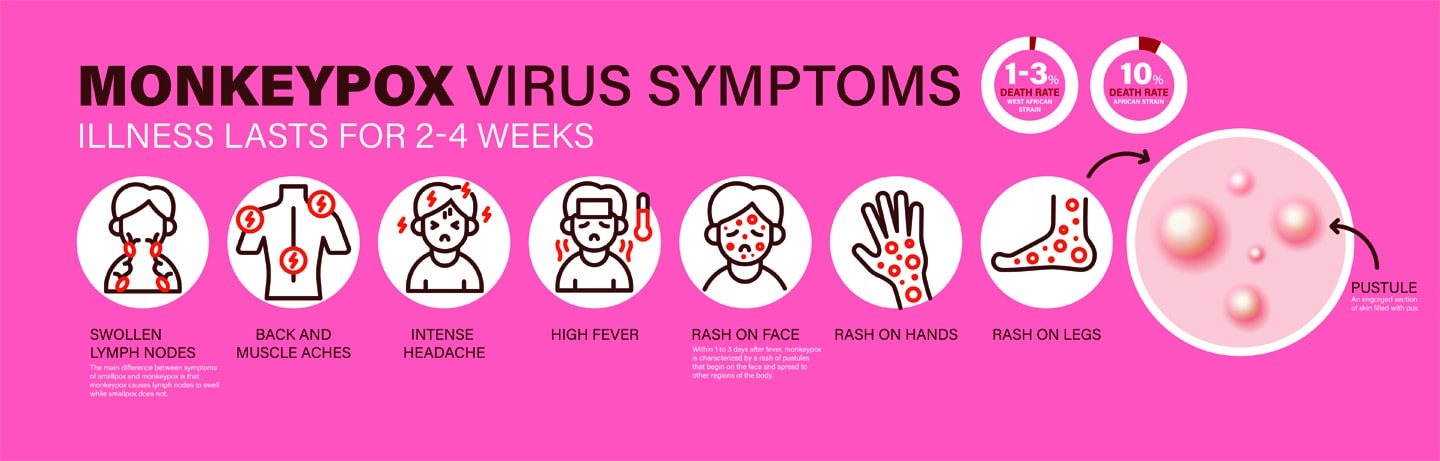
Unlike SARS-CoV-2, which spreads through tiny air-borne droplets called aerosols, monkeypox is thought to spread from close contact with bodily fluids, such as saliva from coughing. That means a person with monkeypox is likely to infect far fewer close contacts than someone with SARS-CoV-2, Hooper says. Both viruses can cause flu-like symptoms, but monkeypox also triggers enlarged lymph nodes and, eventually, distinctive fluid-filled lesions on the face, hands and feet. Most people recover from monkeypox in a few weeks without treatment.
On May 19th, researchers in Portugal uploaded the first draft genome of the monkeypox virus that was detected there, but Gustavo Palacios, a virologist at the Icahn School of Medicine at Mount Sinai in New York City, emphasizes that it’s still a very early draft, and more work needs to be done before any definitive conclusions can be drawn.
What researchers can tell from this preliminary genetic data is that the strain of the monkeypox virus found in Portugal is related to a viral strain predominantly found in West Africa. This strain causes milder disease and has a lower death rate — about 1% in poor rural populations — compared with the one that circulates in Central Africa. But exactly how much the strain causing the current outbreaks differs from the one in West Africa — and whether the cases popping up in various countries are linked to one another — remains unknown.
Answers to those questions could help researchers to determine whether the sudden uptick in cases stems from a mutation that allows monkeypox to transmit more readily than it did in the past, and whether each of the outbreaks traces back to a single origin, says Raina MacIntyre, an
infectious-diseases epidemiologist at the University of New South Wales in Sydney, Australia. Unlike SARS-CoV-2, a rapidly evolving RNA virus whose variants have regularly eluded immunity from vaccines and prior infection, monkeypox is caused by a relatively large DNA virus. DNA viruses are better at detecting and repairing mutations than RNA viruses, which means it’s unlikely that the monkeypox virus has suddenly mutated to become adept at human-to-human transmission, MacIntyre says.
‘Deeply Concerning’
Still, for monkeypox to be detected in people with no apparent connection to one another suggests that the virus might have been spreading silently — a fact that Andrea McCollum, an epidemiologist who heads the poxvirus team at the US Centers for Disease Control and Prevention in Atlanta, Georgia, calls “deeply concerning”.
Unlike SARS-CoV-2, which can spread without causing symptoms, monkeypox does not usually go unnoticed when it infects a person, in part because of the skin lesions it causes. If monkeypox could spread asymptomatically, it would be especially troubling, because it would make the virus harder to track, McCollum says.
Another puzzle is why almost all of the case clusters include men aged 20–50, many of whom are men who have sex with men (MSM). Although monkeypox isn’t known to be sexually transmitted, sexual activity certainly constitutes close contact, Rimoin says. The most likely explanation for this unexpected pattern of transmission, MacIntyre says, is that the virus was coincidentally introduced into an MSM community, and has continued circulating there. Scientists will have a better idea of the origin of the outbreaks and the risk factors for infection once an epidemiological investigation — which can take weeks and involves rigorous contact tracing — is complete.
Containment Strategies
Scientists have been keeping an eye on monkeypox ever since an eradication campaign for smallpox, a closely related virus, wound down in the 1970s. Once smallpox was no longer a threat thanks to worldwide vaccinations, public-health officials stopped recommending smallpox inoculation — which also kept monkeypox at bay. With each year that has passed since smallpox’s eradication, the population with weakened or no immunity to these viruses has grown, MacIntyre says.
There have been a few monkeypox outbreaks since then. The Democratic Republic of the Congo, for example, has been grappling with the virus for decades, and Nigeria has been experiencing a large outbreak, with over 500 suspected and more than 200 confirmed cases, since 2017, when the country reported its first case in some 40 years. The United States also reported an outbreak in 2003, when a shipment of rodents from Ghana spread the virus to pet prairie dogs in Illinois and infected more than 70 people.
Public-health authorities are not powerless against monkeypox. As a precaution against bioterrorism, countries such as the United States maintain a supply of smallpox vaccines, as well as an antiviral treatment thought to be highly effective against the virus. However, the therapies probably wouldn’t be deployed on a large scale to tackle monkeypox, McCollum says. Health-care workers would probably instead use a method called ‘ring vaccination’ to contain the spread of the virus: this would vaccinate the close contacts of people who have been infected with monkeypox to cut off any routes of transmission.
On the basis of the data that she has seen so far, McCollum thinks the current outbreaks probably won’t necessitate containment strategies beyond ring vaccination. “Even in areas where monkeypox occurs every day,” she says, “it’s still a relatively rare infection.”
Source: www.nature.com, by Max Kozlov


